Disclaimer: This blog is written based on our study that has not been accepted by the mainstream yet. We do not intend to replace the advice and consultation of a medical doctor. We invite you to examine the study and discuss it with your doctor before acting on it. The company claims no financial interest for the potential benefit of the information and assumes no responsibility for any adverse results due to improper use of the data.
We May Finish the Pandemic with Fewer Fatalities This Summer by Raising the Curve
(We did not write this blog to promote AllerPops that cannot treat or prevent airway infection, including COVID-19. The author hopes this information will help you to get through this pandemic with fewer difficulties. The author is a former medical doctor and a biologist.)
With all the talk of flattening the coronavirus pandemic curve of infections, we can also ask the question another way: When should we raise the curve?
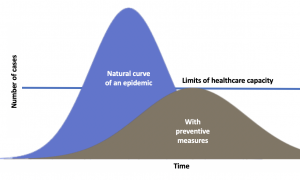
This accompanying chart is one we’re all used to by now: showing the number of newly infected people during a pandemic. The CDC is currently trying to flatten the curve with preventive measures so that the COVID-19 pandemic will not overwhelm the health care system. Today, I will present an alternate option of raising the curve at the right time, which could be a lifesaver. The right time is from late spring to the end of summer when the high temperature will make the pandemic mild with less fatality.
Why does the flu epidemic become mild in warmer season?
Common sense tells us that the flu and common cold occur more in the winter. They do not entirely disappear in the summer, but only exist as a very mild form. The mild epidemic has two aspects — slower progress and lowers death rate. The traditional explanation of why the common cold and flu happen more in the winter is that we stay indoors more in winter and have more chances to catch the virus from each other. However, this explanation does not justify the lower death rate.
Our recent study develops a Theory of Negative Trigger that can explain the seasonal changes of the flu very well. You may read the article at this link: https://allerpops.com/oral-probiotic-deficiency-may-cause-common-allergies/.
Probiotic is the brake (negative trigger).
Our immune system is like a car with an accelerator to speed it up and brakes to slow it down. Pathogens stimulate(speed up) the immune system so it can protect us from diseases, and probiotics (friendly bacteria) slow it down when there is no infection. Like the car, the brake — our probiotics keep our immune system parked most of the time.
The optimal growth temperature for the probiotics in the upper airway is between 85-98°F. Our average body temperature is at the top end of the optimal range. When we are in hypothermia, the temperature shifts to the middle of the spectrum, which may help the bacteria grow better and send too many pacifying messages to the immune system. With an increase in signals from the probiotics, our immune system becomes jeopardized. Without enough baseline protection, the virus that causes the common cold, flu, and very likely coronavirus has a better chance to multiply and cause trouble. This mechanism may contribute to other chronic airway infections, such as chronic bronchitis.
My personal story is a testimony of the theory.
When I was growing up in China, we lived in a house with no heat. Both of my grandparents had severe chronic bronchitis in all their lives, especially in winter. The condition was so critical that it eventually contributed to their deaths. My mom also suffered from chronic bronchitis up until she was fifty. When we moved into a house in the city with heat, her infection went away. Her recovery seemed like a miracle, but it was merely the result of staying warm in the winter.
Therefore, the seasonal flu epidemic becomes mild in the summer is because our defense system in the airway is more robust. With a more vigilant immune system, the population is less susceptible to the virus and less sick when infected.
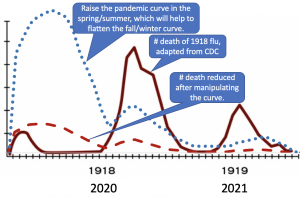
The 1918 flu pandemic fits our theory well.
The 1918 flu pandemic had three-waves. The second and third waves were more lethal. People suggested a virus mutation to blame for that change, but I don’t buy it. One of the first groups to be infected with the 1918 flu was a troop of soldiers. In March of 1918, 1100 soldiers in a Kansas camp caught the virus with a fatality rate of 3.5%, a bit higher than the final 2.5%. So the virus at the beginning was likely as deadly as it was in the second wave. It appeared mildly only in between. Our theory can explain the behavior of the 1918 flu quite well without the imaginary mutation.
The temperature is the key.
The deployment of the troops spread the flu virus to Europe in April 1918, which governmental restrictions prevented its reporting. By the time it reached Spain and was reported in May, the weather had changed. The warmer temperature inhibited human airway probiotics and strengthened its defense system. Patients could then clear the virus more efficiently after an infection. The health care system was relatively sufficient, with fewer patients in serious condition. The warm weather alleviated the outcome, which is likely why the observed first wave was less lethal.
The population became less susceptible to the virus with the summer coming. The first wave eventually became so low in August, that people thought the pandemic to be over. As the temperature dropped in the fall of 1918, the second wave came. Compared to the first wave, the second wave landed mostly in colder temperatures that made the population more susceptible to the virus and sicker when infected. The medical system strained by World War One was overwhelmed with thousands of patients with severe infection. The temporary medical tents located in the cold might have had an increased toll on life as well.
This theory could also explain two sideline stories.
The theory can also explain the unusual W shaped fatality rate. The regular flu caused more death in young children and seniors, but the second wave of the 1918 flu increased the death rate between ages 20-40. More young people, with an average of 26 years old, participated in WWI than other age groups. Young men and women were likely a major supporting force as well. Most war activities happened outdoors, exposing participants to cold weather, which made them more susceptible to flu infection.
Finally, the second sideline story, aspirin toxin, matches the theory too. In 1917, the patent for aspirin expired, and the drug became widely available at a low price. Without much to treat the cause of the 1918 flu, doctors used aspirin to treat the fever to comfort their patients. The dose used is currently considered too high and likely caused severe side effects. In addition to the toxin, the premature return to normal temperatures added another layer of frost to the snow. The lower temperature invited the probiotics back to the airway. The later sent a peaceful signal to the immune system while the infection was still there, which jeopardized the battle against the flu virus.
Sadly, this symptom treatment has become a norm since then. I have written several blogs about the benefit of moderate fever, which is a symptom that is commonly treated immediately in modern times. Please read them here.
Does COVID-19 behave the same as the common cold and flu, and will it become mild in the summer?
We cannot currently examine the question thoroughly as it is still in its early stage, but different progressions of COVID-19 in countries/regions of varying climates may provide clues. Before showing you the data, I should say that various reasons may cause different outcomes in each country/region. The reasons may include population structure, baseline health condition, economic condition, health care capacity, pandemic control measures, social-cultural limits, and many more. Here I approach the question with the lens of temperature impact, which is a warmer temperature increases airway defense and reduces the population’s susceptibility. The result is a pandemic with a slower progression and lower death rate.
New Zealand and Australia
Recently, New Zealand, following Australia, announced a one-month lockdown. I curiously checked their numbers and found: 200 cases and 0 deaths in New Zealand and 2,364 cases and eight deaths in Australia on March 23. The death rate in the two countries is below .4%, which is half to one-twentieth of the scale in other countries. Australia and New Zealand are at the end of their summer or early fall. The pandemic in the region is a lot milder than it is in Europe, China, and the US.
Of course, New Zealand and Australia have their unique situations. Australia has been testing robustly. They may have the highest per capita testing rate in the world. Let’s consider other warm regions much more significant than those two countries and also consider Europe, where it is cold. Europe has a population of 741 M and 575,108 cases of COVID-19, with a fatality rate of 7.4% on April 2, 2020.
The warm and cold continents
South America has a total of 422 M people and 21,378 infected cases with a fatality rate of 3.2%. Africa, with a population of more than 1,216 M, has only 7,237 cases with a death rate of 4.2%. Pandemic in these two continents started later with a slower progression and lower death rate than it did in Europe. Other factors may cause part of the difference. However, both South America and Africa have had warmer weather since the beginning of this pandemic than Europe has.
The smaller countries: Korea and Singapore
Finally, let’s compare COVID-19 in Korea and Singapore. Both countries have many things in common. They got their first cases before the closure of Wuhan. They have been using rigorous and practical approaches to control the epidemic, resulting in a similar total number of sickness relevant to their population. The significant difference is that Korea, where it has been colder, has almost a three times higher death rate (1.7% and .5%) than Singapore.
We may conclude after these comparisons that COVID-19 behaves similarly to the common cold and flu and becomes mild in warm seasons/regions. What should we do if the climate can change the course of the epidemic this dramatically?
The proposal: Raise the curve to save lives this summer.
Before an emergency landing, a necessary preparation to avoid a crash is to dump the fuel. The fuel in this pandemic is the susceptible portion of the population who have no immunity to this virus.
To reduce population susceptibility, we can immunize more people naturally by speeding up the epidemic where/when the fatality rate is low. Currently, this approach could be tested in countries in their wormer seasons. With the reduced sensitivity to the virus, we will flatten the curve and save lives in the coming winter when the fatality rate will be high.
Two fundamentals support this proposal. We have discussed the biological reason for a mild pandemic outcome in the warmer season, and the other one is that COVID-19 will spread all year long before the population becomes immunized, naturally, or through vaccination. The vaccine is at least 12 months away if anything currently being tested works. Locking the world down for a year, which will cause economic and social disasters, is likely not a good option. Alternatively, another option is to raise the curve in the spring/summer so that we can get through the pandemic quickly with a smaller loss of human life.
COVID-19 will most likely continue to spread until the majority of the population is immunized, naturally, or through vaccination.
In China, there was only a tiny window of time to wipe out this virus at the beginning and prevent a pandemic. The dramatic move would have needed to occur around the end of last year. Stopping the epidemic after that time became unrealistic. Several observations justify this “pessimistic”/realistic view.
First, the virus is quite contagious.
Calculations of the virus’s primary reproduction number, or R0 — the number of people on average one infected person will pass the virus to — suggest a range of 2-2.5 (a later revision to be 5.7). As a comparison, R0 for the seasonal flu is between .8-2.2 and that for the 1918 pandemic flu was 1.4-2.8.
Second, the asymptomatic infection.
People can carry the virus for a long time without symptoms and spread it to other people at a lower rate. At the beginning of the epidemic in China, a woman developed flu symptoms and tested positive for the virus 41 days after moving out of Wuhan before its shutting down. Right after Wuhan relaxed its shutdown, an asymptomatic virus carrier caused a doctor to become infected. These asymptomatic carriers are not rare, as reported by NPR.
Third, the virus can survive in the environment for quite a long time.
Depending on the temperature and the texture of the surface, coronavirus can stay alive for hours to days. Researchers detected the COVID-19 virus RNA in cabins of the Diamond Princess cruise ship 17 days after the rooms vacated, though they did not verify that the RNA was from a living virus.
Fourth, no herd immunity.
At this time, finding a new host is easy for the virus since almost all people do not have immunity to it, and this is why COVID-19 can spread in the warm region as well.
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, said on April 5 that the virus is unlikely to be eradicated from the planet this year, and it may come back next flu season. I would say there will very likely be a visible circulation of the virus even in the summer before a significant portion of the population has immunity against the COVID-19 virus. We should not wait for another disaster to happen in the coming fall. We can manipulate this mild summer epidemic for our benefit.
Raise or flatten the curve appropriately for fewer fatalities.
Most countries are trying to flatten the curve so that the health care system will not be overwhelmed, which is the right move for countries where it is winter. Each nation should relax or strengthen their measures according to their medical capacity. Unfortunately, this rarely happens. Many countries try to use the most robust measures they have to crush down the pandemic as much as possible.
Raise the curve from mid-late spring to the end of the summer when the death rate is low so that more people become immunized. Then the curve will be flattened in the fall/winter automatically when the death rate is likely to be higher. This approach will have a much smaller impact on normal life and the economy than other alternatives.
With a better understanding of the pandemic, I hope each country can tailor their response to reduce the damage and, at the same time, have the vast majority live a relatively healthy life. In general, we should tighten the measure to flatten the curve in the fall/winter and relax the means to raise the curve in the spring/summer with the same goal in mind: get through the pandemic with less time and fewer fatalities. (see figure on the right)
How many lives can we save with this approach?
This question is tough to answer. I cannot give you any number close to reality. Based on the current pandemic data around the world, it may save 50% – 90% of the fatalities.
You can help to save these innocent lives by choosing what you can do from the following list:
- Share this proposal with your family and friends through your social media.
- Please write a letter to your congressman or senator and encourage them to examine this proposal.
- Send the blog to your local newspaper.
- Give the proposal to your state/local health official and discuss it with them.
Besides saving lives directly, this approach will give some breathing room to the economy and indirectly support countries and save lives as well. We may finish the pandemic by the end of this summer if we speed the epidemic enough and produce sufficient herd immunity against the virus.
God is not done with you yet.
When I started my car this morning, this song I have heard many times was playing on the Family Life Radio:
…
It’s not over, it’s only begun
So don’t hide, don’t run
‘Cause God’s not done with
You-ou-ou-ou-ou
You-ou-ou-ou-ou
There’s a light you don’t notice
Until you’re standing in the dark
And there’s a strength that’s growing.
Inside your shattered heart
…
So let’s face it. Let’s examine this and other innovative ideas with great potential, make a plan, and act on it now. Together, we can beat this coronavirus.